European “ImmunAID” project for the diagnosis of rare autoinflammatory systemic diseases launched in Belgium
 Monday, January 25, 2021 at 3:08PM
Monday, January 25, 2021 at 3:08PM The project wishes to diagnose rare autoinflammatory systemic diseases through the identification of biomarkers
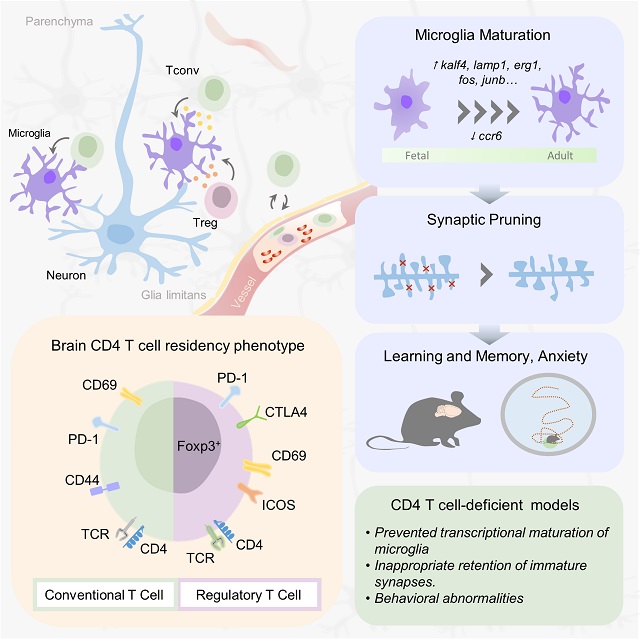
In December 2020 a new project has been launched in the University Hospitals Leuven. The ImmunAID project aims to identify new tools for the diagnosis of systemic auto-inflammatory diseases (SAID). SAID are a complex and evolving group of rare diseases characterised by extensive clinical and biological inflammation. These conditions are caused by a dysregulation of the innate immune system leading to a release of immune cells and mediators provoking fevers, tissue and organ inflammation and damage.
Sometimes it is difficult for the physicians to make a correct diagnosis, since the main symptoms of these diseases (such as fever, rash, joint pain, etc.) are also present in many other conditions. Thus, a patient may have received on average up to 5 inappropriate or ineffective treatments before being properly diagnosed, having a great impact on their health and quality of life. The aim of ImmunAid is to understand the mechanisms that drive the pathology in order to provide better diagnosis and care for patients with these rare but potentially devastating diseases.
An unprecedented body of clinical and biological data in the field of SAID
This new project aims to find new and more effective ways to diagnose SAID. While it is already known that some SAID are due to specific genetic mutations, a large number of SAID can only be detected by a set of clinical signs and symptoms and after other diagnostic possibilities have been excluded. Since SAID are rare conditions, a large group of patients suffering from various SAID is being recruited throughout Europe. As such, the ImmunAID cohort represents a very important tool for researchers defining biological fingerprints, or biomarkers, specific to distinct SAID.
The team expects to find a set of biological features common to all SAID, which will allow to quickly confirm or refute the diagnosis of suspected autoinflammatory syndrome. In addition, for each SAID, a list of characteristic biomarkers and an algorithm will be generated to allow the physician to make an appropriate diagnostic assessment.
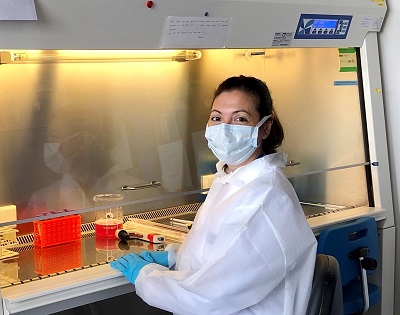
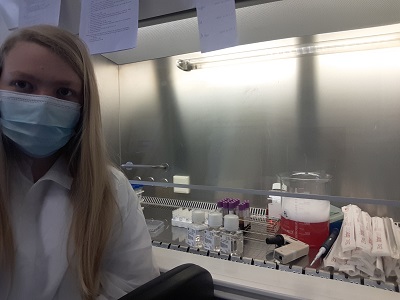
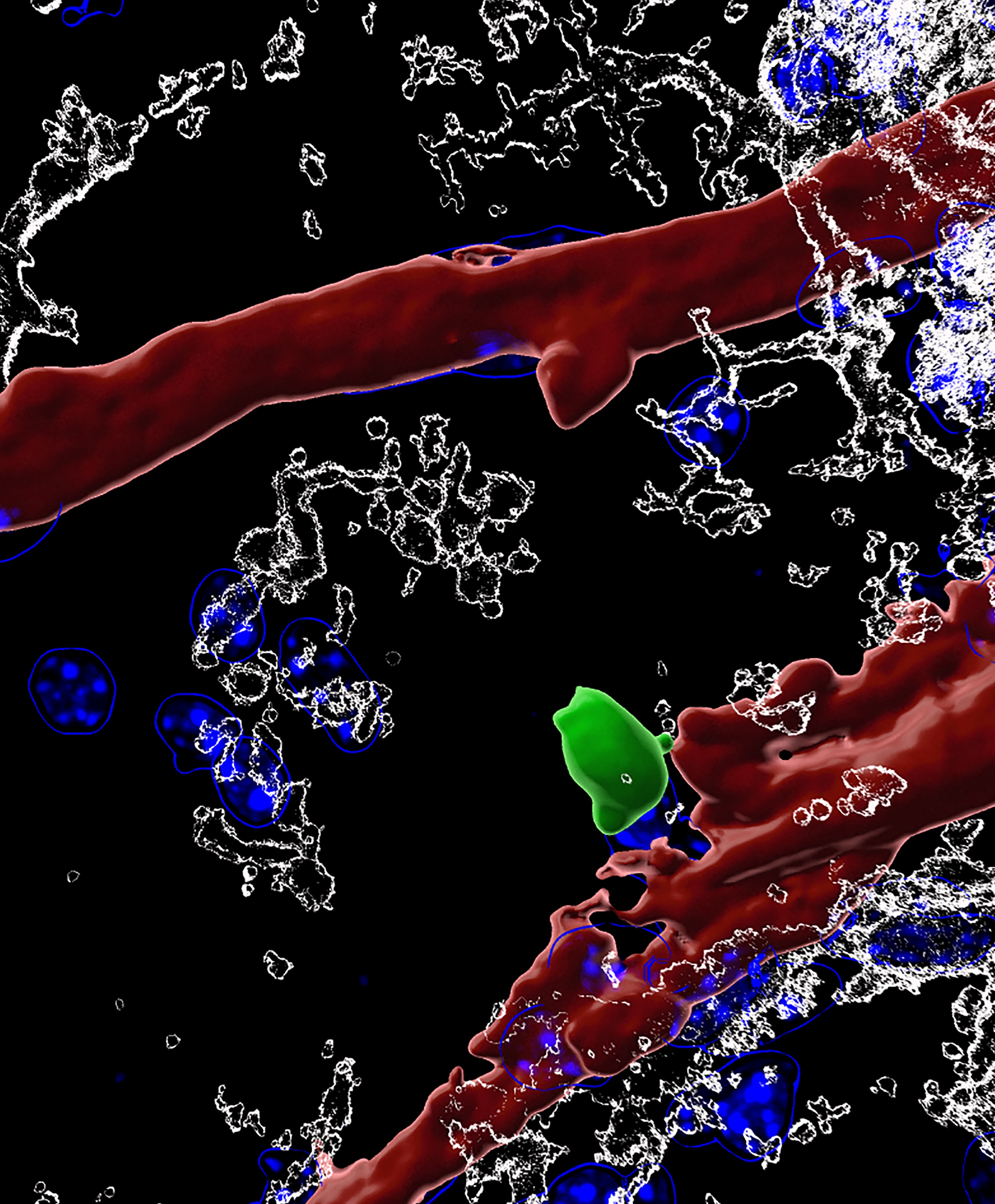
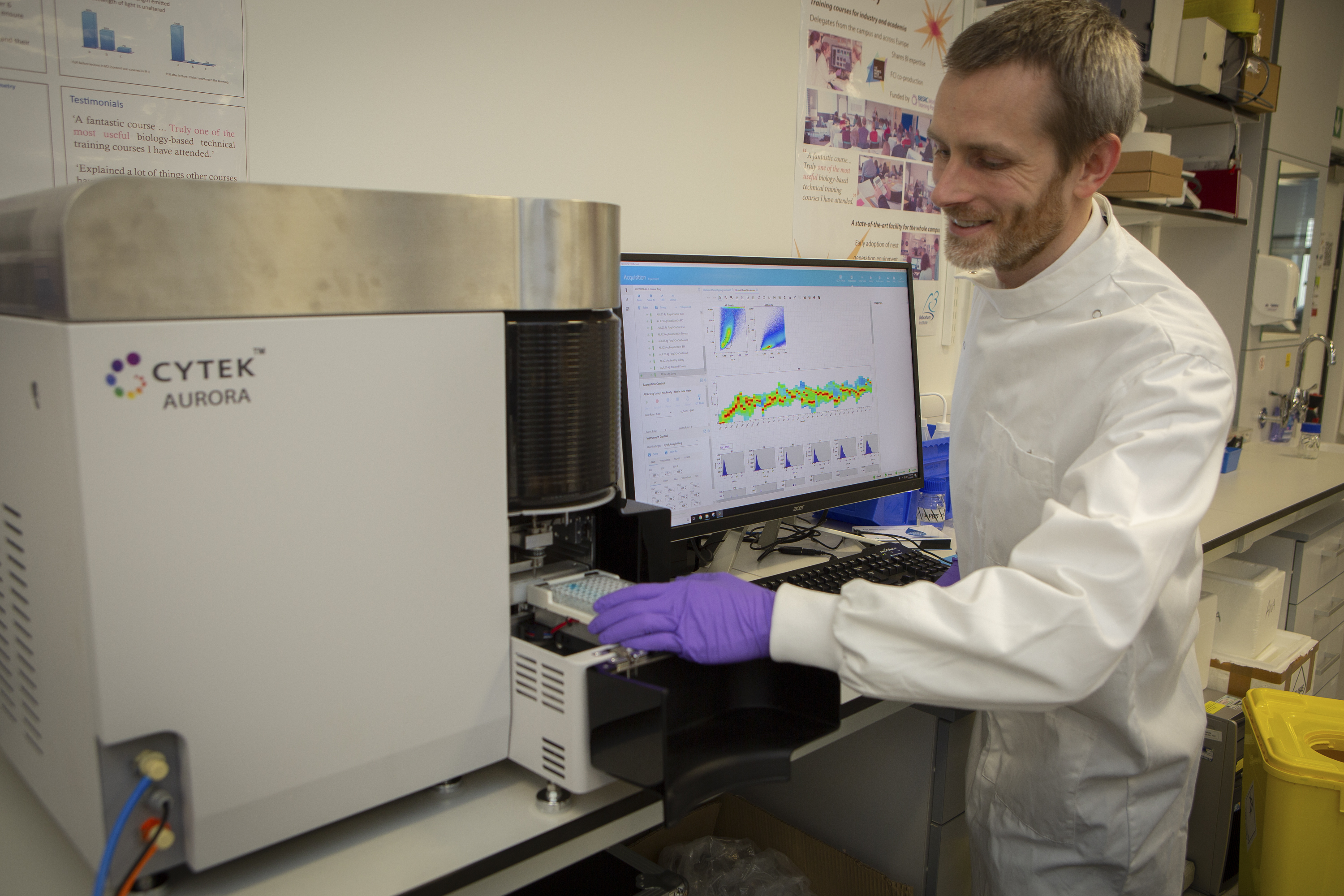
In order to achieve the project's objectives, biological samples collected from the patients will be analysed in a European-wide research network by set of state-of-the-art technologies and will generate an unprecedented amount of data (genomics, transcriptomics, proteomics and microbiome). Simultaneously, other analyses will focus on immune cells, molecular mechanisms and specific agents of the immune system (cytokines, etc.). All data generated will be subjected to artificial intelligence and modelling analysis.
Prof. Carine Wouters, paediatric rheumatologist at the University Hospitals Leuven, is highly committed to the success of the project "We are delighted and proud to be able to work with ImmunAID partners as it represents a unique opportunity for the European scientific community to advance research in an important field of rare diseases that can only be tackled at large scale. We will do our best to come up with meaningful results that will improve patients’ diagnosis and medical care.”
Leuven teams are the forefront of the project
The teams of the Leuven University Projects are at the forefront of the project. The activities carried out in the Belgian centre will be two-fold. First, the team from professor Carine Wouters and professor Steven Vanderschueren will be in charge of recruiting patients suffering from monogenic SAID (FMF, CAPS, TRAPS, MKD) or genetically-undiagnosed SAID (Still disease, neutrophilic dermatosis, Schnitzler syndrome, Takayasu arteritis, Kawasaki disease, Behçet disease, chronic osteitis, recurrent pericarditis and chronic systemic inflammation of unknown origin).
Second, professor Wouters, professor Patrick Matthys and professor Paul Proost from the Rega Institute and KU Leuven department for Microbiology, Immunology and Transplantation will be involved in the biochemical and biological analysis of the samples. The team of Carine Wouters and Patrick Matthys will apply their extensive knowledge on Natural Killer cells to identify and characterize their possible altered activity in SAID patients. On the other hand, the team of Paul Proost will study whether modifications of messengers of the immune system (cytokines and chemokines) in patients play a role in regulation of the inflammation processes. The team of professor Stephanie Humblet-Baron and professor Adrian Liston will analyse in-depth the immune cellular compartment of the blood of affected patients in addition to genetic investigation in order to identify new genes responsible for SAID.
These activities are intended to gain insight into the mechanisms triggering the aberrant behaviour of the autoinflammation process. The results will be pooled with other analyses from other European research laboratories to help identify biomarkers of the diseases and possible therapeutic interventions.
Regarding the ImmunAID project: ImmunAID is a research project (www.immunaid.eu), which aims to identify a set of disease-specific biomarkers to confirm the diagnosis of SAID. ImmunAID is implemented by a large consortium (25 partners in 12 European countries) and has been funded with € 15.8 million by the European Commission. The ImmunAID project has received funding from the European Union's Horizon 2020 research and innovation programme under Grant Agreement No. 779295.
 Liston lab,
Liston lab,  Medicine,
Medicine,  immunology
immunology